Home › Forums › Periodontology › Periodontal Disease
Welcome Dear Guest
To create a new topic please register on the forums. For help contact : discussdentistry@hotmail.com
- This topic has 45 replies, 7 voices, and was last updated 22/01/2013 at 3:55 pm by
 drmithila.
drmithila.
-
AuthorPosts
-
17/05/2010 at 2:56 pm #9208
sushantpatel_doc
OfflineRegistered On: 30/11/2009Topics: 510Replies: 666Has thanked: 0 timesBeen thanked: 0 timesAt one point everyone has seen a little blood in their mouth when brushing their teeth. But bloody gums are not natural and are usually an indicator of an unhealthy mouth.
Red and swollen gums that have a tendency to bleed easy are often a sign of gingivitis. Gingivitis is the inflammation of the gums, which is most often caused by a buildup of bacterial plaque at the gum line. The plaque will continually build up if not cleaned away and can mineralize into tartar, which can further irritate the gums and cause tooth decay. Gingivitis can also be caused by injuries to the gum by brushing too hard or flossing wrong or even sometimes by pregnancy or diabetes. Gingivitis is the most common form of periodontal disease (“gum disease”) and if left untreated, can lead to a more serious form of periodontal disease: periodontitis. Periodontitis is the most advanced stage of periodontal disease and is characterized by the gums receding away from the teeth, leaving open pockets between the teeth and gums. The gums as well as the inner bones progressively receive more and more damage until the teeth become loose and fall out.
To treat mild forms of periodontal disease, healthy eating and daily brushing and flossing are suggested. Dentists may also recommend specialized toothbrushes that are more effective in removing plaque and toothpastes like Colgate Total that contain triclosan which help reduce plaque and gingivitis. Dentists can also prescribe mouth rinses containing chlorhexidine to combat the disease. If the patient is suffering from periodontitis and the teeth are loose, dentists will use the method of scaling and root planing (SRP). Scaling is a process where the dentist scrapes the plaque and tartar off the gum line and then uses root planing to smooth any coarse areas in the roots where bacteria may collect. This helps loose gums reattach to teeth and is used most often incongruence with the antibiotic Periostat, which combats enzymes that hurt both the teeth and gums. There are also other antibiotics that can be placed inside open pockets in the gums such as Atridox (doxycycline hyclate), PerioChip (chlorhexidine gluconate), and Arestin (minocycline) which help close the gaps and reduce bacteria. Dentists though are weary of overusing these antibiotics to treat forms of periodontal disease because there is an increased risk of bacterial resistance to these drugs.
Around 80% of Americans suffer from some form of periodontal disease, but it can be prevented by flossing and brushing everyday as well as visiting a dentist twice a year for a regular cleaning and check-up.
18/05/2010 at 12:35 pm #13826divyanshee
OfflineRegistered On: 24/04/2010Topics: 25Replies: 38Has thanked: 0 timesBeen thanked: 0 times18/05/2010 at 5:30 pm #13827Anonymous
Even there are several etiologies for gingival overgrowth; usually each etiology has its own overgrowth characteristics. For example, while genetically induced gingival overgrowth show firm, normal coloured (pink), non-inflamed gingival tissues, gingival overgrowth due to blood dyscrasias are edematous, soft, tender to touch and show tendency to bleed.
20/05/2010 at 12:35 pm #13828Anonymous
Drug induced gingival overgrowth
The clinical features of gingival enlargement usually presents as enlarged interdental papillae and resulting in a lobulated or nodular morphology. The effects normally limited to the attached and marginal gingivae and more frequently observed anteriorly. Histologically, in drug induced gingival overgrowth it was described as thickening of the spinous cell layer, slight to moderate hyperkeratosis, fibroblastic proliferation and fibrosis of lamina propria .
20/05/2010 at 5:25 pm #13829sushantpatel_doc
OfflineRegistered On: 30/11/2009Topics: 510Replies: 666Has thanked: 0 timesBeen thanked: 0 times20/05/2010 at 6:00 pm #13830shreya
OfflineRegistered On: 14/05/2010Topics: 11Replies: 36Has thanked: 0 timesBeen thanked: 0 times21/05/2010 at 1:27 pm #13831sushantpatel_doc
OfflineRegistered On: 30/11/2009Topics: 510Replies: 666Has thanked: 0 timesBeen thanked: 0 times22/05/2010 at 7:07 am #1383222/05/2010 at 12:42 pm #13833sushantpatel_doc
OfflineRegistered On: 30/11/2009Topics: 510Replies: 666Has thanked: 0 timesBeen thanked: 0 times11/12/2011 at 4:38 pm #14961 drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 times
drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 timesLOCAL DELIVERY OF SITE-SPECIFIC ANTIMICROBIAL DRUGS
The local delivery of antimicrobials, such as Arestin (Orapharma), offer the dentist a statistical and significant system for the treatment of periodontitis.18 The Agency for Health Care Research and Quality (the federal agency assigned to improve quality, safety, efficiency, and effectiveness of healthcare) evaluated literature on these antimicrobials in 2004.19 They concluded that scaling/root planing, when accompanied by the placement of an antimicrobial agent (Arestin) as a supplement or adjunct treatment, resulted in an improved clinical outcome in adults with chronic periodontitis. (This was compared to scaling/root planing that was done alone.) Systemic and locally placed antimicrobial drugs are therefore suggested for use when active disease is detected. They have clearly shown in the studies mentioned to be of significant help in resolving the diseased condition and restore periodontal health as quickly as possible.
Patients usually understand medical treatment with medication. It is a natural addition to periodontal treatment, following the medical model. These drugs can be used on a routine basis as a standard of care, in successfully managing periodontal disease.ROLE OF PROBIOTICS IN MANAGING PERIODONTAL DISEASE
Periodontal disease may be impacted by the use of new probiotic products, such as GUM PerioBalance (Sunstar Americas) and Evora Plus (Oragenics). Probiotics consist of microorganisms in oral tablet/lozenge form that confer a health benefit to the patient. Current research has indicated that periodontal disease may be impacted by probiotics through the reduction of the body’s inflammatory mediators. Twetman et al20, in 2009, using 2 strains of Lactobacillus reuteri, found that there was a reduction in bleeding on probing and the amount of cytokines present in the gingival crevicular fluid, a reduction in the periodontal inflammatory response. This may help to reduce oral disease. GUM Perio Balance is designed to be used once daily, immediately following flossing and brushing. The lozenge dissolves in the mouth in 10 minutes, and it is recommended that nothing be used in the mouth immediately after the use of the lozenge for 30 minutes (Figure 3).11/12/2011 at 4:38 pm #14962 drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 times11/12/2011 at 4:39 pm #14963
drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 times11/12/2011 at 4:39 pm #14963 drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 times
drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 timesPAINLESS MANAGEMENT OF DISEASE
One barrier to consumer acceptance of even conservative nonsurgical periodontal treatment is still the fear of pain. Treatment must be provided painlessly, if at all possible. In order to achieve this, analgesia must be used. It has been estimated that 15% of the US population declines dental care primarily because they fear oral injections.23 Nitrous oxide/oxygen analgesia relaxes patients and reduces their anxiety enough to allow treatment without pain. New technology allows the use of digital flow meters, such as the Porter Instrument Conscious Sedation Flowmeter. To achieve a successful result, analgesia must be available for the patients who require it. A recent innovation (developed by the author) using topical anesthetic spray (such as Hurricane [Beutlich Pharmaceutical]) and a light-cured extended contact topical fluoride varnish (such as Vanish XT [3M ESPE]), makes it possible to perform scaling/root planing without having to use injectable local anesthetics. Previously sensitive roots, which could only be instrumented after administering local anesthetic, can now be treated after a single application of Vanish XT. After being light-cured, the fluoride varnish seals the roots with a durable layer of protection, thus relieving dentinal hypersensitivity and permitting the painless instrumentation and removal of all deposits. Being able to control root sensitivity, while improving the integrity of the root of the tooth where the toxic bacteria collects, gives the dentist/hygienist the opportunity to help control the risk of disease. Reduction of this sensitivity via an extended contact topical fluoride varnish (that can last up to 6 months) can also help to improve patient compliance for performing the required at-home daily hygiene routine; thus making it easier to control the chronic disease risks and improving the future success of dental care.
16/12/2011 at 2:44 pm #14983Drsumitra
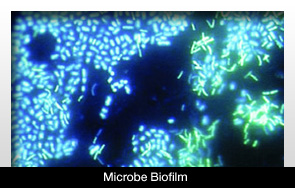
OfflineRegistered On: 06/10/2011Topics: 238Replies: 542Has thanked: 0 timesBeen thanked: 0 timesnew type of fluorescent labeling technology determined that microbe biofilm can interact with other bacteria when located on a tooth.
It was determined that a single image can demonstrate some type of cooperation between the various forms of microbe biofilm.
The information was revealed during a presentation at the American Society for Cell Biology meeting in Denver.
The specific types of bacteria that interacted were Prevotella and Actinomyces. The study to figure out the roles bacteria play in the mouth was conducted by a research team from the Marine Biological Laboratory.
Prevotella is the bacteria often associated with periodontal disease. There have also been cases in which the bacteria were present in anaerobic lung infections.
This new technology will lead to several other new findings involving bacteria. It could be pivotal to research involving tooth decay or any other dental problem related to bacteria
16/12/2011 at 2:46 pm #14984Drsumitra
OfflineRegistered On: 06/10/2011Topics: 238Replies: 542Has thanked: 0 timesBeen thanked: 0 times10/04/2012 at 5:48 pm #15375 drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times
drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 timesA primary aim of periodontal probing is to locate the most coronal level of the connective-tissue attachment. However, this generally is not attainable, as penetration of the probe tip in the pocket or the lining soft tissues correlates with periodontal health.7,8 It has been established that the extent of probe penetration is influenced by the inflammatory status of the tissues.7,9-12 In most instances when healthy tissues are examined, the probe tip stops coronal to the apical termination of the junctional epithelium (Figure 1), whereas at inflamed sites the probe tip frequently passes apical to this point (Figure 2). The depth of probe penetration partially depends on the extent to which the gingival connective tissue has been lysed or infiltrated by inflammatory cells. In other words, intact connective tissue underlying the crevicular epithelium is an important factor resisting probe penetration. Spray et al13 suggested that the state of health of the underlying connective-tissue fibers influences probing measurements. There is a “hammock effect” in health, where healthy fibers act as a barrier and prevent apical movement of the instrument, while inflamed connective tissue offers less resistance to penetration. With reduction in inflammation, an accurate estimate of the sulcus depth is more likely to be obtained. The probe penetration is significantly greater in the presence of visible inflammation, but not where there was bleeding after probing.8 These results suggest that the location of the inflamed connective tissue may be a critical factor. Anderson et al14 determined the correlation between clinical and histologic inflammation and probe-tip penetration of the pocket tissues in dogs. A strong correlation was found between probe penetration and degree of inflammation, and the difference in mean inflammation scores between sites where probes were located coronal or apical to the epithelium was statistically significant.
Anatomically, the gingival sulcus is defined as the distance from the gingival margin to the coronal extension of the junctional epithelium.15 However, the ability of the periodontal probe to measure this distance accurately is questionable. Results of human studies performed by Sivertson and Burgett16 indicate that the periodontal probe routinely penetrates to the coronal level of the connective tissue attachment of untreated periodontal pockets. Armitage et al7 found that, in healthy specimens, the probe failed to reach the apical termination of the junctional epithelium. In cases with experimental gingivitis, however, most probes came closer to the apical termination of the junctional epithelium, but on the average still fell short. In periodontitis specimens, the probes consistently went past the most apical cells of the junctional epithelium. A significant relationship between the degree of inflammation and level of probe penetration was found. Saglie et al17 noted that probing depths measured in the laboratory were always shallower than those recorded clinically. The authors attributed this discrepancy to the presence of a zone of completely and partially destroyed periodontal fibers, which allowed the probe to extend apically to the coronal level of connective-tissue attachment. The results of these studies illustrate that periodontal probes do not precisely measure, and often overestimate, the true histologic sulcus depth, and that inflammation has a significant influence on probe penetration. This has important implications regarding how measurements taken with periodontal probes are interpreted. Because probes rarely stop at the exact location of the most apical cells of the junctional epithelium, probing measurements are clearly not precise assessments of the actual level of connective-tissue attachment. PPD measurements overestimate connective-tissue attachment loss at inflamed sites and underestimate it at noninflamed sites. An increased probing depth is a sign of reduced tissue resistance to probing, which in turn can be interpreted as an indication of the presence of an inflammatory cell infiltrate in the gingival tissue.11Most research has shown that the tendency for penetration of the probe into the tissues at the base of pocket resulting in an overestimate of probing depth is greater at inflamed sites7,10,11 and in nonsmokers
-
AuthorPosts
- You must be logged in to reply to this topic.