Home › Forums › Endodontics & conservative dentistry › Phase Format Treatment for Endodontic Therapy
Welcome Dear Guest
To create a new topic please register on the forums. For help contact : discussdentistry@hotmail.com
- This topic has 2 replies, 2 voices, and was last updated 13/04/2012 at 5:25 pm by
Anonymous.
-
AuthorPosts
-
13/04/2012 at 5:22 pm #10449
Anonymous
OnlineTopics: 2Replies: 1153Has thanked: 0 timesBeen thanked: 2 timesPhase Format Treatment for Endodontic Therapy
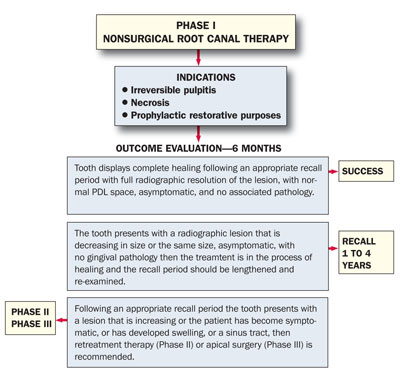
Figure 1. Phase I: Nonsurgical root canal therapy outcome assessment flow chart. INTRODUCTION
Current trends in endodontic therapy aim to more adequately disinfect the root canal system. The introduction of nickel titanium rotary instruments has allowed a more efficient debridement of the canal and expel pathogenic debris coronally rather than apically.1,2Activated irrigation regimens of 5.25% NaOCl, 17% EDTA, and 2% chlorhexadine have also been shown to penetrate biofilms and inaccessible areas of the root canal system to achieve disinfection.3-6 Additionally, magnified visualization with microscopes has allowed detection and differentiation of previously unobserved morphology. Current microsurgical endodontic procedures with ultrasonic preparation and biocompatible retrofillings have also significantly improved treatment outcomes compared to traditional techniques.7-10 These advancements have allowed the modern trend of evaluating early endodontic treatment success at 6 months to one year.11-13 However, retrospective evaluation of more modern techniques have shown that a longer recall period may allow continued healing, and that late periapical changes in endodontically treated roots resulted in more successes than failures. Even with this current knowledge, the criteria used to evaluate endodontic treatment success and failure dates back to the 1950s and 1960s. In 1956, Strindberg developed strict radiographic criteria in which the contours and width of the periodontal ligament were normal or widened around excess filling material and a failure was a decrease, no change, or increase in the periradicular rarefaction. Bender18 went on to publish a reappraisal of endodontic success criteria in 1965 that highlighted the pitfalls of radiographic interpretation, recall period, pathology and patient and provider subjectivity. Seltzer19,20 built upon this in 1967 and concluded that since there is no agreement of a definition of success, then regardless of radiographic interpretation, endodontically treated teeth which are functioning adequately without adverse clinical symptoms should be regarded as successfully treated. Nonetheless, the criteria used to evaluate modern endodontic treatment needs to reflect current trends.
The purpose of this paper is to introduce a phase format treatment outcome assessment guideline that incorporates current knowledge of endodontic therapy success.PHASE FORMAT ENDODONTIC THERAPY
Endodontic therapy consists of and progresses from initial root canal therapy, root canal retreatment, and apical surgery. The phase format will provide an outline for clinicians to exhaust all treatment options prior to determining the tooth inoperable. The field of periodontics introduced this concept of presenting a phase format treatment plan as an entire unit in which Phase I is nonsurgical, Phase II is surgical, Phase III is restorative, and Phase IV is maintenance.21
The field of endodontics needs to expand upon this design and present treatment as an entire unit. By presenting endodontic procedures as an overall therapy to achieve success, it becomes apparent that each phase of the treatment is completed to provide a foundation for rehabilitation. Each stage of treatment will be evaluated independently, but the assessment of treatment failure should not be concluded prior to progressing through the phases of therapy. Endodontic therapy is intended to achieve results within the confines of the treatment provided in the same fashion that retreatment therapy and apical surgery are evaluated within the parameters of their outcome expectations.13/04/2012 at 5:25 pm #15388Anonymous
PHASE I—Nonsurgical Root Canal Therapy Indications
Phase I of the outcome assessment guideline (Figure 1) involves initiating endodontic therapy according to various clinical, radiographic and patient subjective findings. Initial endodontic therapy including and/or progressing from pulpotomy, pulpectomy, apexogensis, apexification, and nonsurgical root canal therapy completing with obturation of root canal should be initiated following a history of patient symptoms and vitality testing indicating irreversible pulpitis, necrosis or prophylactic restorative purposes. The tooth should be deemed restorable according to current prosthetic standards. Initial endodontic therapy should be thorough but conservative in nature, maintaining a favorable restorative prognosis.
Outcome Evaluation
The evaluation of Phase I therapy should include and be confined to the expectations of the initial root canal therapy. First, if the tooth displays complete healing following a 6-month recall with full radiographic resolution of the lesion, with a normal periodontal ligament (PDL) space, asymptomatic, and no associated pathology, then the case can be considered a success. Second, if the tooth presents with a radiographic lesion that is decreasing in size or the same size, asymptomatic, with no gingival pathology, then the treatment is in the process of healing and the recall period should be lengthened to one to 4 years and be re-examined for complete healing. Third, if following an appropriate recall period the tooth presents with a lesion that is increasing or the patient has become symptomatic, or has developed swelling, or a sinus tract, then retreatment therapy (Phase II) or apical surgery (Phase III) should be recommended. At this stage of the treatment, the initial root canal therapy should be evaluated and an assessment of the treatment quality should be obtained. If the instrumentation and obturation appears that it can be improved and is accessible, then retreatment therapy should be recommended. If the instrumentation and obturation appear to be adequate and the accessibility of retreatment is difficult due to natural or iatrogenic blockage, then apical surgery should be recommended. The therapy should not be considered a failure at this point if the initial instrumentation and obturation appear to follow current standards, rather a building block toward achieving endodontic therapy success.PHASE II—Nonsurgical Retreatment Therapy Indications
Phase II of the outcome assessment guideline (Figure 2) involves initiating nonsurgical retreatment root canal therapy following the evaluation of previous therapy, healing and patient symptoms. Retreatment of initial endodontic therapy is indicated if the patient presents symptomatic, demonstrates swelling, or displays a fistula tract indicative of a persistent or secondary infection. Retreatment is also indicated if the endodontic filling material has been exposed to the oral environment for an extended period, making it susceptible to reinfection. The tooth should again be deemed restorable according to the current prosthetic standards. Retreatment of the root canal system attempts to address the conservative nature of initial root canal therapy and more aggressively pursues additional canals and enlarges the instrumentation to adequately detoxify the root canal system.
Additionally, the provider assessing the case may be unaware of the conditions under which the initial root canal therapy was performed and should aspire to complete the retreatment under current aseptic and technical standards. In addition to modifying the instrumentation, additional irrigation regimens along with fluid agitation can be used to address resistant microbial communities. Lastly, an optimal obturation following current material standards and techniques can be placed to resist leakage.Outcomes/Evaluation
The evaluation of Phase II therapy should include and be confined to the expectations of the retreatment root canal therapy. First, if the tooth displays complete healing following a 6-month recall period with full radiographic resolution of the lesion, with a normal PDL space, asymptomatic, and no associated pathology, then the case can be considered a success. Second, if the tooth presents with a radiographic lesion that is decreasing in size, asymptomatic, functional with no associated pathology, then the treatment is in the process of healing and the recall period should be lengthened to one to 4 years and be re-examined for complete healing. Third, if following an appropriate recall period the tooth presents with a lesion that is increasing or the same size, the patient has become symptomatic, or has developed swelling, or a sinus tract, then apical surgery (Phase III) should be recommended. At this stage of the treatment, the endodontic therapy should be evaluated and concluded that the root canals are adequately instrumented and obturated and no improvement can be accomplished. Once again, the therapy should not be considered a failure at this point if the initial or retreatment instrumentation and obturation appear to follow current standards; rather, a building block toward achieving endodontic therapy success.13/04/2012 at 5:25 pm #15389Anonymous
PHASE III—Apical Surgery Indications
Phase III of the outcome assessment guideline (Figure 3) involves initiating one or all services involving manipulation of the roots including apical surgery, apical resurgery, perforation repair, root amputation, hemisectioning, intentional reimplantation, exploratory surgery. The patient may demonstrate a radiographic lesion that has not adequately healed or describe persistent symptoms with an associated pathology. The tooth in question may also demonstrate inaccessible areas of the root canal system that could not be instrumented safely due to natural, iatrogenic, or restorative blockage. The goal of radicular surgery is to mechanically remove pathology and optimally seal the defect to promote healing. Phase III relies upon current surgical techniques that address etiological factors beyond initial and retreatment root canal therapy. All teeth treatment planned for surgical intervention should be thoroughly examined for proper preoperative and postoperative prosthetic rehabilitation prior to initiating therapy.
Outcomes/Evaluation
The evaluation of Phase III therapy should include the final evaluation of endodontic therapy success or failure. First, if the tooth displays complete healing following a 6-month recall period with full radiographic resolution of the lesion, with a normal PDL space, asymptomatic, and no associated pathology, then the case can be considered a success. Second, if the tooth presents with a radiographic lesion that is decreasing in size, asymptomatic, functional with no associated pathology then the treatment is in the process of healing and the recall period should be lengthened to one to 4 years and be re-examined for complete healing. Third, if the patient is asymptomatic and the lesion appears smaller but persistent over a lengthened period of time, a scar formation may be considered and the therapy a success. Fourth, if following an appropriate recall period the tooth presents with a lesion that is increasing or the same size, the patient has become symptomatic, or has developed swelling, or a sinus tract, then apical resurgery or extraction should be recommended.
Following this exhaustive process of providing all therapy accessible prior to determining the tooth inoperable, the therapy should now be considered unsuccessful. Each phase of endodontic therapy addressed its specific goals, and if the tooth remains symptomatic or demonstrates increased bony destruction, then the therapy should be considered a failure and an alternative prosthetic replacement should be considered.SUMMARY
This paper has shown that modern endodontics has progressed significantly in describing and treating pulpal and periradicular pathology. Current knowledge indicates that endodontic therapy should be evaluated as a complete unit and that each phase of treatment is completed to provide a foundation for rehabilitation. The phase format assessment of endodontic therapy success provides an outline for clinicians to objectively provide treatment in effort to conserve natural dentition. -
AuthorPosts
- You must be logged in to reply to this topic.