Home › Forums › Sleep Dentistry › Snoring Treatable By Dental Device
Welcome Dear Guest
To create a new topic please register on the forums. For help contact : discussdentistry@hotmail.com
- This topic has 9 replies, 5 voices, and was last updated 17/05/2012 at 5:09 pm by
Drsumitra.
-
AuthorPosts
-
03/11/2011 at 5:47 pm #10093
 drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 times
drsushant
OfflineRegistered On: 14/05/2011Topics: 253Replies: 276Has thanked: 0 timesBeen thanked: 0 timesA physician, Dr. Smith (not his real name), mentioned at his dental visit that he snores heavily and that recently his condition has been diagnosed as obstructive sleep apnea. Dr. Smith said that he had read that a certain kind of dental device can treat this condition and wanted to know whether he is a suitable candidate.
Sleep apnea occurs where there are episodes of cessation of breathing lasting 10 seconds or longer during sleep. The failure to breath triggers the brain to awaken briefly in order to reinitiate the breathing process. These arousals are so brief that they generally go unremembered. But the results of these frequent interruptions are daytime sleepiness, which may lead to disruption of work and social life. Difficulties with concentration, memory are some of the other symptoms. Severe sleep apnea may lead to high blood pressure, heart failure, heart attack and stroke.
Sleep apnea is estimated to affect about of 10% men between the ages of 30 to 50, but also has been found in both sexes of all ages. The most frequent form of sleep apnea is obstructive sleep apnea, in which the cessation of breathing is most often caused by excessive relaxation of the muscles at the back of the throat.
Dr. Smith was aware that medical remedies include the use of continuous positive airway pressure (C- PAP) which involves the use of wearing a mask over the nose and mouth. Air from a compressor forces air through the mask to keep the airway open. Surgical procedures involve the excising of excess tissue at the back of the throat, such as enlarged tonsils and adenoids. However Dr. Smith cannot sleep with the C- PAP mask and does not want surgery. He was interested in the mandibular advancement appliance that has been used to treat obstructive sleep apnea.
This dental device consists of two retainer-like plastic covers. One fits over the upper teeth and the other over the lower teeth. These two retainers are joined together by “connectors” which maintain the lower jaw slightly more forward than normal. By advancing the lower jaw (mandible) forward, the diameter of the throat is increased. More importantly, even if the muscles at the back of throat relax, the throat is prevented from collapsing. This forward placement of the mandible can prevent the blocking of breathing found in obstructive sleep apnea.
A mandibular advancement device was made for Dr. Smith. A subsequent polysomnograph (sleep study) confirmed that while Dr. Smith was wearing the oral device, he had no apnea episodes. His “oxygen saturation rate” was back to normal and he felt great. The snoring has greatly diminished to where it is almost not noticeable to his wife. He has continued to wear this kind of appliances for the past four years.
If you or your spouse suffers from the snoring of the other, there is hope. Visit your dentist. If you also notice that he/she has apnea episodes where breathing stops for 10 seconds or more, please see your physician to rule out sleep apnea. If you have sleep apnea, be sure you follow your doctors’ instructions as to how to deal with this condition. Ask your physician if a mandibular advancement device could be a consideration.
12/12/2011 at 10:46 am #14966Anonymous
Though snoring is general, this condition can hurt relationships and make difficult to sleep apnea, a sleeping chaos characterized by a silence in breathing for a least amount of 10 seconds several times in a single night, and in turn can lead to additional serious health problems similar to heart ailments, hypertension, high blood pressure and stroke according to current studies.
____________________
12/12/2011 at 4:39 pm #14971abhijitbagalkot
OfflineRegistered On: 12/12/2011Topics: 0Replies: 1Has thanked: 0 timesBeen thanked: 0 times12/01/2012 at 12:40 pm #15064Anonymous
14/03/2012 at 4:40 pm #15276 drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times
drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 timesWithin the past 10 years, there has been a huge increase in the diagnosis and treatment of sleep disorders, such as obstructive sleep apnea (OSA), by the medical community. Because there are many patients who are unable to tolerate continuous positive airway pressure (CPAP) therapy (Figure 1) prescribed by medical doctors, dentistry has a tremendous new opportunity to help patients in the treatment of sleep disorders. The American Academy of Sleep Medicine (AASM) has designated dental sleep appliances as the top nonsurgical alternative for the CPAP intolerant patient. In addition, in February of 2006, the AASM designated dental sleep appliances to be a viable treatment for mild to moderate sleep apnea.1 This has opened the door for dentists who are trained to treat snoring/mild-moderate sleep apnea, and who want to help CPAP intolerant patients.
Dentists now have more advanced appliance choices for sleep breathing disorders. The purpose of this article is to introduce an example of a new concept in sleep therapy using a single-arched mandibular (or maxillary) oral appliance. In addition, it is important to note that we have better techniques for diagnostics and the fitting of these appliances, including the use of 3-dimensional (3-D) dental imaging. Using such techniques, dentists are capable of achieving high success rates consistently with their snoring and CPAP-intolerant patients.
SNORING
Snoring is caused by a restriction in the size of the airway with rapidly moving air vibrating the tissues in the oropharyngeal airway. If the tongue is restrained from closing the airway, the snoring dissipates.
Fifty-two percent of all Americans age 40 years or older snore.2 Twenty-seven percent of all couples more than 40 years old sleep apart because of snoring problems. A recent article in the Wall Street Journal stated that new housing construction was beginning to include 2 master bedrooms in new homes.3 In fact, the problem of bothersome snoring within households has become so widespread that separate sleeping quarters are frequently desired.
Without a reliable and broad-based remedy in use, snoring has become a ubiquitous American cultural phenomenon.14/03/2012 at 4:40 pm #15277 drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times
drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 timesCONTINUOUS POSITIVE AIRWAY PRESSURE: HIGHLY SUCCESSFUL, HIGHLY REJECTED

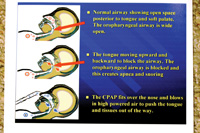
Figure 1. Patient sleeping using continuous positive airway pressure (CPAP) therapy.
Figure 2. Diagrams show how CPAP functions.
After weight loss, the number-one medical treatment for snoring and OSA is CPAP therapy. It is an extremely successful treatment modality for these problems. (Figure 2 shows how the CPAP device functions.)
However, CPAP therapy presents its own difficulties since it is not tolerated by 50% to 60% of the patients who are treated with it.4,5Some of these difficulties include dry/stuffy nose, irritated facial skin, sore eyes, and headaches. If the CPAP device is not properly adjusted, the patient may get stomach bloating and discomfort while wearing the mask. Without the ability to wear the CPAP device, these patients are left to “fall through the cracks” untreated. Where do they go, and what hope do they have for the successful treatment of their condition?ORAL SLEEP APPLIANCES


Figure 3. The Tap appliance, an example of a double-arch appliance that opens the bite and positions the mandible/tongue forward. Figure 4. The SUAD appliance, another example of a double-arch appliance.

Figure 5. Tongue-retaining appliance that holds the tongue forward with suction.
The answer for people who are CPAP intolerant lies with dental sleep appliances. In the proper diagnosis and use of oral sleep appliances, dentistry has a workable solution for sleep apnea and snoring. With this, dentistry has been handed a major responsibility in the treatment of snoring and OSA.
For the most part, the dental devices currently available for the treatment of snoring and OSA are double-arched appliances. Success is achieved by opening the vertical dimension and advancing the mandible forward.6 The advancement can be from edge-to-edge to, as much as, a full protrusive position. With some patients, the vertical is opened as much as 10 to 15 mm. In this way, the tongue is pulled forward and the airway opened.
Two popular double-arched sleep appliances that advance the mandible and open vertical are illustrated in Figure 3, the Tap appliance, and Figure 4, the SUAD appliance.
Another option is the tongue-retaining device (Figure 5). It holds the tongue forward by suction, created when the tongue is inserted into a rubber bubble in the front of the appliance.
Appliances like these can be successful, however, a large percentage of them can be uncomfortable since mandibular advancement can lead to jaw pain, changes in occlusion, and tempromandibular disease problems. Furthermore, what can be done once the dentist has opened the vertical, and moved the jaw forward as far as possible, without accomplishing the reduction of snoring and apneic events? The treatment is finished, unsuccessfully.SINGLE-ARCHED APPLIANCES
In September, 2006, a new maxillary single-arch oral sleep appliance was introduced to dentistry called the Full Breath Solution (FBS). It allows the clinician to take a very different approach to treatment. Rather than pulling the tongue forward by advancing the mandible, it works by utilizing a “tail” that restrains the tongue from moving upward and backward. The tail is expanded posteriorly and inferiorly, depressing the tongue in the same manner in which the medical doctor utilizes a wooden tongue blade in an exam. The tongue is gently depressed in order to open and view the airway. In the same way, dentists can utilize the tail on the single-arch FBS oral appliance to open the airway.
In June, 2009, the mandibular single-arch FBS oral appliance was granted FDA certification, and subsequently introduced into patient care. This was the fifth FDA certification granted to the FBS appliance since 2004.
The CPAP is almost 100% successful, when tolerated, because the positive pressure of the continuous air stream pushes the tongue forward keeping the airway open. Similarly, the FBS oral appliance is successful because it depresses and restrains the tongue, inhibiting the tongue from moving up/backward and blocking the airway. An oral device that controls the tongue is able to control and open a patient’s airway, allowing more oxygen to enter the lungs, dramatically improving nighttime breathing.

Figures 6a and 6b. Single-arch maxillary Full Breath Solution (FBS) appliance.


Figure 7. The tail of the lower FBS which can be seen here depresses the tongue and prevents it from moving posteriorly.
Figure 8. An underside view of a mandibular FBS appliance. Two to 4 clasps are placed for retention.
Figures 6a and 6b show the maxillary FBS oral appliance, and Figures 7 and 8 show the mandibular FBS oral appliance. The mandibular FBS single-arched appliance utilizes a posterior tongue restrainer (PTR), or “tail” to depress the tongue.
The FBS appliance gains its clinical success by small additions of acrylic to get posterior and inferior extension of the PTR (tail). This allows for more leverage in restraining the tongue. The formation of the tail, which acts exactly like a tongue depressor, prevents the tongue from its upward and backward movement resulting in an open airway and reduced/eliminated snoring.

Figure 9. Blue wax has been added to the tail of the maxillary FBS appliance.
Figure 10. Blue wax has been added to the tail of the mandibular FBS appliance.


Figures 11 and 12. Wax has been removed and replaced with cold-cured acrylic to the same approximate shape both a maxillary and a mandibular FBS. The tails can now function like a tongue depressor to open the airway.
With either the maxillary (Figure 9) or mandibular appliance (Figure 10), wax is incrementally added to the tail, a little at a time, to clinically test for patient comfort and tolerance. If comfortable, the wax is removed and acrylic is added in the same approximate size and shape as the wax-up (Figures 11 and 12). In this way, the tail is expanded (from its original lab-fabricated starting point) to adequately depress the tongue.
Depression can be slight, or much deeper, depending on the patient. The question that invariably comes up is the comfort of the tail. Approximately 5% of patients complain of discomfort or irritation. In those cases, the tail is cut off. Then, approximately 3 weeks later, the tail is added back on in small increments of acrylic extensions. This approach produces a uniform success rate with patients (breathing and comfort) in the 99th percentile. When desired, acrylic can also be removed from the superior surface of tail to keep it thinner and more comfortable.
Despite the tail, the properly fabricated and adjusted FBS appliance will not cause gagging. The reason lies with the physics and effects of snoring. When a person is snoring, the tongue falls back and closes the airway from 80% to 90%. As the air flows through the constricted airway, it picks up speed as it moves through the reduced opening. This constantly speeding air desensitizes the nerve endings on the posterior section of the tongue. As a result, there is a reduction or elimination of the normal gagging reflex due to a reduction of tactile nerve endings on the tongue.14/03/2012 at 4:45 pm #15278 drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times
drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times3-D IMAGING
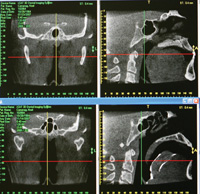
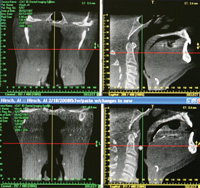
Figure 13. In these CAT scan views, the lateral cervical view (upper right) shows the small airway caused by the posterior position of a large tongue. The lower right image is the same individual with the FBS appliance in place. Figure 14. These images show the increase in the size of the airway achieved with the FBS appliance. Compare the pretreatment image (upper right) with the post-treatment (lower right) image. Again, note the tongue depressing effect of the tail to depress the tongue and open the airway.
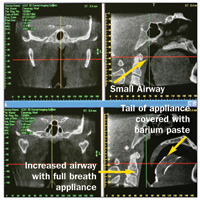
Figure 15. In the upper right, the superior posterior tip of the tail is touching the soft palate and can be a cause of discomfort. Also, the tail needs to be repositioned downward to better control the tongue. The lower right image shows the changes made to the appliance and the increased airway.
The tail, which is the key to successfully treating the patient, is incrementally elongated and thickened in depth until the snoring is eradicated. The elongation of the tail with acrylic is done by adding a little length and slowly increasing the depth inferiorly, gauging clinical success by the lack of snoring. The pace of addition is based on the comfort/tolerance of the patient with each addition.
The most efficient and precise method of increasing tail size is provided by one of dental radiology’s new diagnostic tools, 3-D cone beam. 3-D imaging allows detailed viewing of appliance tail placement, tongue position, and the size of the airway. It also makes precise adjustments possible to maximize the airway opening. We can easily analyze how and where we should add acrylic to the tail to maximize the opening of the airway. We are able to observe the original restricted airway, and then to see the improved airway with use of the FBS appliance. 3-D dental imaging clearly illustrates the ability of the appliance’s tail to control the tongue and open the airway (Figures 13 to 15)14/03/2012 at 4:45 pm #15279 drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 times
drmithila
OfflineRegistered On: 14/05/2011Topics: 242Replies: 578Has thanked: 0 timesBeen thanked: 0 timesCASE EXAMPLES: USINGTHE FBS ORAL APPLIANCE
CASE 1
A 31-year-old male patient presented with a history of severe snoring, moderate sleep apnea, and resulting fatigue. The patient had been previously treated with somnoplasty and an uvuloectomy, resulting in only minimal improvement. CPAP had been prescribed by the medical doctor, but the patient was found to be CPAP intolerant.
Treatment would consist of a pretreatment PSG (lab or hospital sleep test) to determine the Apnea Hypopnea Index (AHI) (the number of times the oropharygeal airway is blocked by the tongue per hour), FBS oral appliance therapy, and a post-treatment AHI.
Including the initial visit, delivery appointment, and subsequent visits to adjust the appliance, treatment consisted of 5 appointments. It was successful in correcting the patient’s sleep problems. AHI went from 33 to 2. (See Figure 16 for the pre-and post-treatment images associated with this case.)CASE 2
A 67-year-old male patient presented with snoring that was disturbing to his wife, and fatigue upon awakening. CPAP therapy had been previously prescribed by his medical doctor and he was found to be CPAP intolerant. Treatment would consist of a pretreatment PSG, FBS oral appliance therapy, and a post-treatment PSG.
Treatment involved 5 appointments and was successful. AHI went from 20.1 to 2.4. (See Figures 17a and 17b for the pre-and post-treatment images associated with this case.)CASE 3
A 67-year-old male patient with a history of severe sleep apnea presented with fatigue and morning headaches. CPAP had been previously prescribed by a medical doctor, and the patient was very unhappy with it, still waking fatigued with morning headaches.
The patient wanted a FBS oral appliance to open the airway so he could reduce the high airflow setting of the CPAP device. Treatment would consist of a pretreatment PSG, a FBS oral appliance therapy with continued use of CPAP, and a post-treatment PSG.
In this case the lateral and frontal views of this patient’s airway appear good-sized. Pretreatment AHI was 109.9. (See Figure 18 for the pre- and post-treatment images associated with this case.) This patient’s sleep study showed that he stopped breathing 109.9 times an hour. Why? The real culprit in OSA reared its head in this case: the tongue was falling back 109.9 times an hour and blocking his airway.
Treatment success was achieved with the FBS appliance. The patient was very happy because he was able to reduce the CPAP airflow needed. His AHI went from a 109.9 (pretreatment) to 22 (post-treatment). This post-treatment AHI represented a large
reduction from the pretreatment AHI using an oral appliance.DISCUSSION
In all 3 of the above cases, controlling the tongue resulted in increased airways and successful results. The oral appliance tail depressed the tongue and prevented the tongue from moving posteriorly to block the airway. This resulted in reduced AHI readings and the elimination of snoring. All 3 cases demonstrated an increase of the oropharygeal airway from the lateral view. In addition, we got a very pleasant surprise when we viewed the frontal view of the same airways: the lateral width of the 3 airways all increased with minimal advancement using the expanded tails of the FBS.CONCLUSION
The best treatment available for OSA is CPAP therapy, but its rejection rate has been estimated by some to run as high as 75%. After weight loss, the best nonsurgical treatment for snoring/OSA is an oral appliance.
The FBS sleep appliance differs from other sleep appliances in that it has a posterior transpalatal/translingual bar and a Posterior Tongue Restrainer (tail). This controls and restrains the tongue in a manner that could not be previously achieved. In addition, utilizing 3-D imaging allows the dentist to view treatment progress and to make the appropriate changes to ensure clinical success. Utilizing these advanced oral and imaging techniques, dentistry can now realize success in treating snoring and OSA patients in the 99th percentile range, far beyond the low tolerance rates of CPAP, and well beyond the hit-and-miss success rate of the mandibular advancing technique.
In the author’s opinion, dentists are now able to offer an option for the treatment of snoring, mild to moderate OSA, and CPAP intolerance, that can dramatically improve the quality
and longevity of life for our patients.17/05/2012 at 5:07 pm #15502Drsumitra
OfflineRegistered On: 06/10/2011Topics: 238Replies: 542Has thanked: 0 timesBeen thanked: 0 timesCentral sleep apnea (CSA) occurs when the brain does not send the signal to breathe to the muscles of breathing. This usually occurs in infants or in adults with heart disease, cerebrovascular disease, or congenital diseases, but it also can be caused by some medications and high altitudes.
Central sleep apnea may occur in premature infants (born before 37 weeks of gestation) or in full term infants. It is defined as apneas lasting more than 20 seconds, usually with a change in the heart rate, a reduction in blood oxygen, or hypotonia (general relaxation of the body’s muscles). These children often will require an apnea monitor that sounds an alarm when apneas occur. Central sleep apnea in children is not the same thing as sudden infant death syndrome (SIDS).
Under normal circumstances, the brain monitors several things to determine how often to breathe. If it senses a lack of oxygen or an excess of carbon dioxide in the blood it will speed up breathing. The increase in breathing increases the oxygen and decreases the carbon dioxide in blood. Some people with heart or lung disease have an increase in carbon dioxide in their blood at all times.
When there is a chronic (long term) increase in blood carbon dioxide, the brain starts to ignore the oxygen level and monitors the blood carbon dioxide level to determine when to take the next breath. The control of breathing also becomes slower to respond to changes in carbon dioxide levels; so when a person takes more or deeper breaths and "blows off" carbon dioxide the drive to breathe decreases and the rate of breathing decreases. As a result of slower rate of breathing, the carbon dioxide builds back up in the blood and the rate of breathing increases again. The brain, slow to adjust, continues to signal for more rapid breathing until the carbon dioxide level drops too low. Breathing then slows down or stops until the carbon dioxide level rises again. This pattern of abnormal breathing is called Cheyne-Stokes breathing (after the men who described it). It is characterized by repetitive cycles of fast breathing followed by slow breathing and apnea. This breathing pattern happens when the person is awake or asleep, but becomes more of a problem when asleep. Some patients with heart failure have central sleep apnea associated with a Cheyne-Stokes pattern of breathing.
Central sleep apnea usually occurs in adults with other medical problems. In infants, it usually occurs with prematurity or other congenital disorders. In both patient groups it is usually suspected by the primary care doctor. Central sleep apnea can be diagnosed with a sleep study or overnight monitoring while the patient is in the hospital.
In infants, central sleep apnea is treated with an apnea alarm. This alarm monitors the infant’s breathing with sensors and sounds a loud noise when the infant experiences an apnea. The alarm usually wakes the infant and the parents. Most infants usually "out-grow" the central apnea episodes, so the alarm monitoring is stopped after the episodes resolve. In infants with other congenital problems, apnea monitoring may be needed for a longer period.
In adults with central sleep apnea, the apneas are treated by treating the underlying heart disease, medication interaction, high altitude, or other primary problem.
Article
Related Diseases
Images & Quizzes
smaller
medium
larger
Previous
1
2
3
4
5
6
7
8
9
10
Next
Sleep Apnea (cont.)What is obstructive sleep apnea and what causes it?
In obstructive sleep apnea (OSA), apneas have four components.
First, the airway collapses or becomes obstructed.
Second, an effort is made to take a breath, but it is unsuccessful.
Third, the oxygen level in the blood drops as a result of unsuccessful breathing.
Finally, when the amount of oxygen reaching the brain decreases, the brain signals the body to wake up and take a breath. (This is what the bed partner hears as a silence followed by a gasp for air.)
First, it is necessary to describe a "normal breath." A normal breath of air passes through the nasal passages, behind the soft palate and uvula (part of the soft palate), then past the tongue base, through the throat muscles, and between the vocal cords into the lungs. An obstruction to the flow of air at any of these levels may lead to apnea. The following are some examples:airflow can become diminished if a person has a deviated septum (the middle wall of the nose that separates the two nostrils). A septum can be deviated to one or both sides narrowing the air passages;
there are filters in the nose called turbinates that can obstruct airflow when they become swollen;
if the palate and uvula (the part of soft palate that hangs down in the back of the throat) are long or floppy, they can fall backwards and close the area through which air flows;
the back of the tongue can also fall backwards and obstruct breathing especially when individuals lay flat on their backs; or
the side walls of the throat can fall together to narrow or close the airway.
To break it down even further:the muscles of breathing work to expand the chest and lower the diaphragm to degenerate a negative pressure between the airways of the lungs and outside;
this negative pressure literally sucks air into the lungs;
the nasal passages, palate, tongue, and pharyngeal tissues can all contribute to narrowing of the airway;
if during an attempt to breathe the airway collapses or is obstructed the tissues of the airway are sucked together by the negative pressure;
the harder the chest tries to pull air in the greater the negative pressure and the more the tissues of the airway are sealed together; and
finally, when the oxygen in the blood stream decreases the person wakes up or the level of sleep becomes more shallow in order to more consciously take a breath.
People with obstructive sleep apnea have an airway that is more narrow than normal, usually at the base of the tongue and palate. When lying flat, the palate is above the air passage. When the pharyngeal muscles (muscles of the pharynx or throat ) relax the palate can fall backwards and this can obstruct the airway.The genioglossus muscle is located where the base of the tongue attaches to the jawbone in front. Most people have enough space behind the tongue to take a breath without needing to pull the tongue forward. However, when obstructive sleep apnea patients are awake, this muscle needs to be active to pull the base of the tongue forward to open the airway. During sleep, most muscles including the genioglossus relax. During the stage of rapid eye movement (REM), the muscles completely relax. Relaxation of the genioglossus muscle during sleep allows the base of the tongue to fall backwards and the airway closes.
Patients with obstructive sleep apnea often don’t report waking up during the night with each episode of apnea. Frequently, during the apnea the brain only awakens from a deep sleep (stages 3, 4, or REM) to a shallow level of sleep. The genioglossus muscle then contracts and pulls the tongue forward so that a breath can be taken. The patient may remain asleep, but the deep sleep that is important to be fully rested the following day is disrupted
17/05/2012 at 5:09 pm #15503Drsumitra
OfflineRegistered On: 06/10/2011Topics: 238Replies: 542Has thanked: 0 timesBeen thanked: 0 timesBehavioral changes are the simplest treatments for mild obstructive sleep apnea, but often the hardest to make. Occasionally, apneas occur only in some positions (most commonly lying flat on the back). A person can change his or her sleeping position, reduce apneas, and improve their sleep.
Obesity is a known contributing factor to obstructive sleep apnea. It is estimated that a 10% weight gain will worsen the apnea-hypopnea index by 30%, and a 10% weight loss will decrease the apnea-hypopnea index by 25%. Therefore, a healthy lifestyle and diet that encourages weight loss will improve obstructive sleep apnea.
Unfortunately, most people with obstructive sleep apnea are tired and do not have much energy for exercise. This is a difficult behavioral spiral since the more tired a person is — the less they exercise — the more weight they gain — the worse the obstructive sleep apnea becomes — and the more tired they become. Frequently, after obstructive sleep apnea is treated by other methods people are able to lose weight and the obstructive sleep apnea may improve.
Sleep hygiene and other behavioral modifications known to improve the overall quality of sleep are also recommended. Below are some common practices that can induce sleep and enhance its quality:
reduce lighting and noise in the bedroom;
avoid reading or watching TV in bed;
avoid eating or exercising prior to sleep;
use the bedroom only for sleeping;
keep work related activities outside of the bedroom; and
try a period of physical and mental relaxation before going to bed.
MedicationMany medications have been studied for obstructive sleep apnea; however, because obstructive sleep apnea is due to an anatomic airway narrowing it has been difficult to find a medication that helps.
In people with nasal airway obstruction causing obstructive sleep apnea, nasal steroid sprays have been shown to be effective. In one study, the respiratory disturbance index (RDI) decreased from 20 to 11 with nasal sprays.
Topical nasal decongestants such as oxymetazoline and neosynephrine, also can temporarily improve nasal swelling. The problem is that they cannot be used for more than 3-5 days without decreased effectiveness and withdrawal symptoms.
People who have obstructive sleep apnea due to hypothyroidism (low thyroid hormone production) improve with thyroid replacement therapy. However, people with normal thyroid function, will not improve with this therapy.
People who have obstructive sleep apnea due to obesity may improve with diet medications if they are effective in assisting with weight loss.
Other medications have been studied, including medroxyprogesterone (Provera, Cycrin, Amen), acetazolamide (Diamox) , theophylline (Theo-Dur, Respbid, Slo-Bid, Theo-24, Theolair, Uniphyl, Slo-Phyllin), tricyclic antidepressants, and selective serotonin reuptake inhibitors (SSRIs). In these studies, they were shown to have little or no effect. There are also new medications to help increase alertness. They may be temporarily successful in increasing attention; however, they do not treat the sleep deprivation or the cause of obstructive sleep apnea.
In cases where sleep apnea may be caused by another underlying condition, appropriate treatment of such conditions is recommended and may be beneficial. For example, treating underlying heart failure may improve sleep apnea if it is a contributing factor. In people with sinusitis and nasal congestion, the swelling and inflammation of the upper airway passages can cause snoring and sleep apnea. Therefore, medications to treat underlying sinusitis and congestion can potentially improve sleep apnea in these individuals.
Medications are also available that could increase daytime wakefulness in people who suffer from sleep apnea. These medications stimulate the brain through an unknown mechanism of action. The prototypical drug in this class is called modafinil (Provigil). Studies have revealed greater resolution of daytime sleepiness when using modafinil in patients with sleep apnea. A similar, newer drug in this class, called armodafinil (Nuvigil), has a longer half-life and is also approved by the FDA for the treatment of excessive daytime sleepiness in people with sleep apnea. Armodafinil has shown similar clinical results in significantly improving daytime quality of life and functioning. It is important to note that the primary treatment for obstructive sleep apnea (OSA) remains CPAP (described below). Stimulants, such as modafinil (Provigil) and armodafinil, are recommended for those who have excessive daytime sleepiness despite proper CPAP use at night. They are not meant to replace CPAP use, but rather, as an adjunctive therapy to CPAP in those who have daytime symptoms even with CPAP use. Approximately one third of people who use CPAP at night for sleep apnea may continue to have somnolence during the day. This is the population that could benefit from using modafinil (Provigil) or armodafinil (Nuvigil).
Dental appliancesA dental appliance holds the jaw and tongue forward and the palate up, thus preventing closure of the airway. This small increase in airway size often is enough to control the apneas.
Dental appliances are an excellent treatment for mild to moderate obstructive sleep apnea. It is reported to be about 75% effective for these groups. A dental appliance does not require surgery; it is small, portable, and does not require a machine. However, there are some disadvantages to the dental appliance. It can cause or worsen temporomandibular joint (TMJ) dysfunction. If the jaw is pulled too far forward, it can cause pain in the joint when eating. For this reason, it is best to have a dentist or oral surgeon fit and adjust the appliance. A dental appliance requires natural teeth to fit properly, it must be worn every night, and the cost is variable, as is insurance coverage.
Continuous positive airway pressure (CPAP)
Continuous positive airway pressure (CPAP) is probably the best, non-surgical treatment for any level of obstructive sleep apnea. In finding a treatment for obstructive sleep apnea, the primary goal is to hold the airway open so it does not collapse during sleep. The dental appliances and surgeries (described later) focus on moving the tissues of the airway. CPAP uses air pressure to hold the tissues open during sleep.
CPAP was first used in Australia by Dr. Colin Sullivan in 1981 for obstructive sleep apnea. It delivers the air through a nasal or face-mask under pressure. As a person breathes, the gentle pressure holds the nose, palate, and throat tissues open. It feels similar to holding your head outside the window of a moving car. You can feel the pressure, but you can also breathe easily.
The CPAP machine blows heated, humidified air through a short tube to a mask. The mask must be worn snugly to prevent the leakage of air. There are many different masks, including nasal pillows, nasal masks, and full-face masks. The CPAP machine is a little larger than a toaster. It is portable and can be taken on trips.
Determining CPAP pressure: With CPAP it is important to use the lowest possible pressure that will keep the airway open during sleep. This pressure is determined by "titration." Titration frequently is performed with the help of polysomnography. It can be performed during the same night as the initial polysomnography or on a separate night. In the sleep laboratory an adjustable CPAP machine is used. A mask is fit to the person and he or she is allowed to fall back asleep.
During baseline sleep the apneas and hypopneas occur, and the the technician then slowly increases the CPAP pressure until the apneas and hypopneas stop or decrease to a normal level. A different pressure may be needed for different positions or levels of sleep. Typically, laying on the back and REM sleep promote the worst obstructive sleep apnea. The lowest pressure that controls obstructive sleep apnea in all positions and sleep levels is prescribed.
Effectiveness of CPAP: CPAP has been shown to be effective in improving subjective and objective measures of obstructive sleep apnea.
It decreases apneas and hypopneas.
It decreases sleepiness as measured by surveys and objective tests.
It improves cognitive functioning on tests.
It improves driving on driving simulation tests and decreases the number of accidents in the real world.
When adjusted properly and tolerated, it is nearly 100% effective in eliminating or reducing obstructive sleep apnea.An important clinical outcome of CPAP use is in the area of prevention of the potential complications of obstructive sleep apnea. Studies have shown that the proper use of CPAP reduces hospitalization for cardiac and pulmonary causes in people with obstructive sleep apnea. More generally, treating obstructive sleep apnea with CPAP can reduce the risks of conditions related to obstructive sleep apnea, such as, ischemic heart disease, abnormal heart rhythms, stroke, hypertension, and insulin dependence.
Problems with CPAP: The first 2-4 weeks is the crucial time to become a successful CPAP user. During this time, it is important to try to sleep as many hours a night as possible with the mask on. If the mask does not fit properly or the machine is not working it is important to have it fixed immediately. It is also helpful to remember all of the increased risks of untreated obstructive sleep apnea (decreased productivity, heart attacks, strokes, car accidents, and sudden death) as an incentive to continue using CPAP.
People with severe obstructive sleep apnea, never get a normal night of sleep. They often put on the CPAP mask and think it is the best thing ever. They quickly get used to it because it allows them to sleep. They take it on vacations because without it they have no energy and are always sleepy.
However, CPAP is not always easy to use. People with only mild to moderate sleep apnea often have a harder time using CPAP. About 60% of people with CPAP machines report that they use them, but only 45% of them actually use them more than four hours per night when the actual use time is measured. Between 25% and 50% of people who start using CPAP, stop using it.
It is not easy to sleep with a mask that is blowing air into your nose. Some people are claustrophobic and have difficulty getting used to any mask. If a patient has nasal congestion or a septal deviation; it is important to have these evaluated since they can be treated (as discussed later). Some people do not like the inconvenience of sleeping with the mask or traveling with the machine. Others do not like the image of having to sleep with a mask. The noise of the machine blowing air can also be bothersome to some people using the CPAP or their bed partners.
Bi-level positive airway pressure (BiPAP)
Bi-level positive airway pressure (BiPAP) was designed for people who do not tolerate the higher pressures of CPAP. It is similar to CPAP in that a machine delivers a positive pressure to a mask during sleep. However, the BiPAP machine delivers a higher pressure during inspiration, and a lower pressure during expiration, which allows the person not to feel like they are breathing out against such a high pressure, which can be bothersome. It is most helpful for people who require a higher pressure to keep their airway open. BiPAP was designed to improve CPAP compliance; however it is difficult to measure an increase in compliance when compared to standard CPAP. BiPAP is often only approved by insurance companies after documentation that a patient cannot tolerate CPAP.
Auto-titrating continuous positive airway pressure
The auto-titrating CPAP machine is a "smart" CPAP machine that makes pressure adjustments throughout the night. As discussed above, different pressures are needed for different levels of sleep and positions. The goal of auto-titrating CPAP is to have the lowest possible pressure for each position or sleep level. At a given pressure, if a person starts to have an apnea or hypopnea, the machine adjusts the pressure higher until the episodes are controlled. If a person is in a sleep level or position that doesn’t need a higher pressure, the pressure is reduced. The benefit is when a lower pressure is all that is required, the machine is not stuck at the highest pressure needed. The down side is, if the machine does not adjust, a person can be stuck at a lower pressure having episodes of sleep apnea.
With auto-titrating CPAP, the mean pressure throughout the night is lower and 2/3 of the night is spent below the set CPAP pressure. The machine also can adjust for the changes in pressure that are needed to overcome the effects of weight gain and alcohol or sedative use. It may also improve compliance; however, this has not been measured. The disadvantages of auto-titrating CPAP are that leaks may underestimate pressure or airflow. Each company has a different algorithm for adjusting the pressure and adjusting for leaks. It is unclear which company has the best algorithm, but studies are on-going.
-
AuthorPosts
- You must be logged in to reply to this topic.